The measurement of end-tidal carbon dioxide (ETCO2) in a hospital setting serves several purposes, including:
Monitoring respiratory status: ETCO2 is a direct measurement of the amount of carbon dioxide being exhaled by a patient, which reflects their respiratory status. Continuous ETCO2 monitoring allows healthcare providers to quickly detect changes in ventilation, airway obstruction, or respiratory distress.
Assessing the effectiveness of ventilation: ETCO2 monitoring is used to assess the adequacy of ventilation during mechanical ventilation, cardiopulmonary resuscitation (CPR), or procedural sedation. It helps healthcare providers ensure that the patient is receiving the appropriate amount of air exchange, and that there is no obstruction in the airway.
Identifying ventilation-perfusion (V/Q) mismatch: ETCO2 monitoring can help identify V/Q mismatch, a condition in which the amount of air reaching the alveoli does not match the amount of blood reaching the same area of the lung. This condition can occur in conditions such as pulmonary embolism and can cause low ETCO2 readings.
Monitoring sedation: ETCO2 monitoring is used to monitor the respiratory status of patients who are receiving sedation or anesthesia, as these medications can cause respiratory depression. By monitoring ETCO2, healthcare providers can detect respiratory depression early and intervene to prevent respiratory failure.
Overall, measuring ETCO2 is an important tool for healthcare providers to monitor and manage patients' respiratory status in a hospital setting.
There are two common techniques used for measuring ETCO2 in a hospital setting:
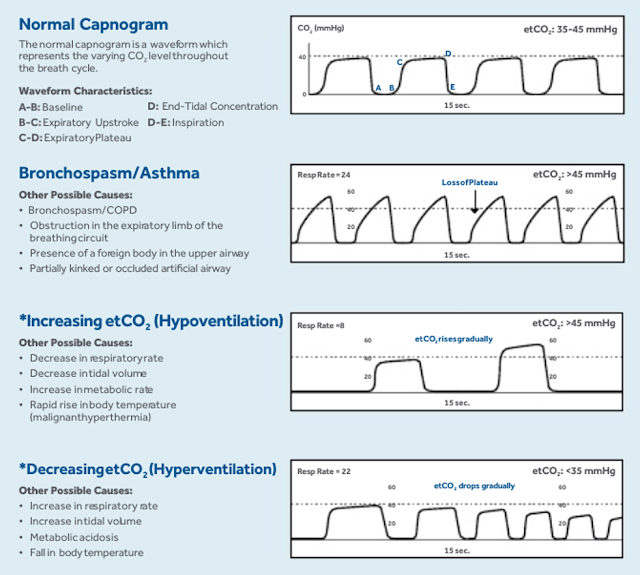
Capnography: Capnography is the most commonly used technique for ETCO2 measurement. It involves attaching a capnography device to the patient's airway (such as a nasal cannula or endotracheal tube) that measures the concentration of CO2 in the exhaled breath. The capnography device provides a waveform graph that displays the ETCO2 level and the respiratory rate. This technique is non-invasive and provides continuous monitoring.
Blood gas analysis: Blood gas analysis is an invasive technique that involves drawing a blood sample from an arterial line and analyzing it for its CO2 level. This method provides an accurate measurement of the partial pressure of CO2 in arterial blood (PaCO2), which is a useful indicator of the patient's overall respiratory status. However, this technique is more invasive and requires blood sampling, which is not as convenient for continuous monitoring as capnography.
Both capnography and blood gas analysis are effective techniques for measuring ETCO2 in a hospital setting. Capnography is non-invasive, continuous, and provides real-time data, making it the preferred method for most situations. Blood gas analysis is more invasive and time-consuming but provides more detailed information about the patient's respiratory status. The choice of technique depends on the patient's condition, the level of monitoring required, and the preferences of the healthcare provider.
In capnography, there are two methods of sampling ETCO2: side stream and main stream.
Side stream capnography: In side stream capnography, a small tube is attached to the patient's airway via a nasal cannula or a mask. The tube draws a small sample of exhaled air from the airway and transports it to the capnography device for analysis. The sample is taken continuously or intermittently, and the results are displayed as a waveform on the monitor. Side stream capnography is typically used in non-intubated patients and in situations where a nasal cannula or mask is being used for oxygen delivery.
Mainstream capnography: In mainstream capnography, a sensor is placed directly in the patient's airway, usually at the endotracheal tube or the tracheostomy tube. The sensor is connected to the capnography device, which continuously analyzes the patient's exhaled breath for CO2 concentration. The results are displayed as a waveform on the monitor. Mainstream capnography is commonly used in intubated patients undergoing mechanical ventilation or during anesthesia.
The main difference between side stream and mainstream capnography is the location of the sensor that measures ETCO2. In side stream capnography, the sensor is located outside the patient's airway, while in mainstream capnography, the sensor is located inside the airway. Both techniques have their advantages and disadvantages and are used in different clinical situations based on patient need, clinical context, and the healthcare provider's preference.
Mainstream capnography sensors are typically more expensive than side stream sensors for several reasons:
Technological complexity: Mainstream capnography sensors are more complex and sophisticated than side stream sensors because they are placed directly in the patient's airway. They require advanced technology and precise manufacturing processes to ensure accurate measurement and reliable performance. This complexity and sophistication contribute to the higher price of mainstream capnography sensors.
Durability and maintenance: Mainstream capnography sensors are placed in a high-stress environment and are exposed to moisture, temperature changes, and other factors that can affect their performance over time. As a result, they require frequent calibration and maintenance to ensure accurate measurement. This increased durability and maintenance requirement also contribute to the higher price of mainstream capnography sensors.
Limited market: Mainstream capnography sensors have a more limited market than side stream sensors because they are primarily used in intubated patients undergoing mechanical ventilation or during anesthesia. This limited market means that there are fewer manufacturers producing mainstream capnography sensors, which can drive up their price.
Overall, the higher price of mainstream capnography sensors is due to their technological complexity, durability and maintenance requirements, and limited market. However, the benefits of using mainstream capnography sensors, such as accurate and continuous monitoring of ETCO2 in intubated patients, make them a valuable tool in critical care settings.
The main blocks of an ETCO2 sensor can vary depending on the type and manufacturer of the device, but generally include the following components:
Sampling chamber: The sampling chamber is the part of the ETCO2 sensor that collects and measures the CO2 concentration in the patient's exhaled breath. In mainstream capnography sensors, the sampling chamber is located directly in the patient's airway, typically at the endotracheal tube or tracheostomy tube. In side stream capnography sensors, the sampling chamber is a separate component that is connected to the patient's airway via a nasal cannula or mask.
Infrared light source: An infrared light source is used to measure the concentration of CO2 in the exhaled breath. The light source emits infrared radiation that is absorbed by the CO2 molecules in the exhaled breath, which generates a signal that is measured by the sensor.
Detector: The detector is the component that measures the signal generated by the infrared light source as it passes through the exhaled breath. The detector measures the absorption of the infrared radiation by the CO2 molecules and converts the signal into an electrical signal that is sent to the capnography device for analysis.
Microprocessor: The microprocessor is the electronic component that processes the electrical signal generated by the detector and converts it into a waveform graph that displays the ETCO2 level and respiratory rate.
Calibration component: ETCO2 sensors require frequent calibration to ensure accurate measurement. The calibration component is used to calibrate the sensor and adjust it for optimal performance.
Overall, the main parts of an ETCO2 sensor are the sampling chamber, infrared light source, detector, microprocessor, and calibration component. These components work together to measure the concentration of CO2 in the patient's exhaled breath and provide accurate monitoring of ETCO2 levels.
One of the Mainstream EtCO2 sensor has broken apart to see the internal components, and it's specifications and relevant details are given below.
EtCO2 Sensor description
EtCO2 Sensor is a mainstream end tidal CO2 Sensor that using advanced dual channel non dispersion infrared absorption spectrum technology. The EtCO2 Sensor is used to monitor continuous carbon dioxide and report the End Tidal carbon dioxide (EtCO2), inspired CO2 and respiratory rate values of the incubated adult, pediatric, infant and neonatal patient. Because of its unique design, response is fast, stability, and excellent price-performance.
Principles of operation
The Mainstream EtCO2 Sensor is used for the continuous measurement of CO2 (carbon dioxide) and respiratory rate. Mainstream EtCO2 Sensor is a non-dispersion infrared analyzer. In Sensor, infrared light is generated by the Sensor and beamed through the sample cell to a detector on the opposite side. CO2 from the patient that is aspirated into the sample cell absorbs some of this infrared energy. The Sensor determines CO2 concentration in the breathing gases by measuring the amount of light absorbed by these gases. The Sensor contains a reference channel, used to compensate for optical changes, so that the system is in a state of calibration. EtCO2 is displayed as a numerical value in millimeters of mercury (mmHg). percent (%), or kilopascals (kPa). In addition, a CO2 waveform (capnogram) may be displayed which is a valuable clinical tool that can be used to assess patient airway integrity and proper endotracheal tube (ETT) placement. Respiration rate is calculated by measuring the time interval between detected breaths.
Preparations for use
This section provides information how to setup the EtCO2 Sensor. Mainstream EtCO2 Sensor is a rugged, solid-state, main stream sensor. It is factory calibrated and does not require further calibration.
Setting up
1. Connect the sensor to the host monitor.
2. Install the airway adapter. Zero the sensor if a message indicating you should calibrate the sensor. Refer to the monitor operator's manual for calibration information.
3. Confirm that the monitor's barometric pressure setting is correct. Refer to the appropriate service manual for information on how to set the barometric pressure.
4 Position the adapter and sensor in the patient respiratory circuit as close to the patient as possible. A location between the endotracheal tube and the ventilator circuit is common.
Warning: Always position the sensor with the adapter in an upright position to avoid collection of fluids on the windows of the adapter. Large concentrations of fluids at this point will obstruct gas analysis.
Combine with the airway adapter
1. Verify the adapter is intact.
2 Make sure the adapter window is dry and clean. 3. Press the Mainstream EtCO2 Sensor onto the airway adapter, it will "click" when properly seated.
4. Make sure the sensor is properly connected to the adapter, and the adapter window is dry and clean.
Install the airway adapter
1. Install at the proximal end of the circuit between the elbow and the ventilator wye. If using an HME, place adapter between HME and wya.
2. The cord of the sensor should be facing away from the patient. 3. For optimal results, do not place the adapter between the ET tube and the elbow.
Zeroing the Sensor
The zero allows the EtCO2 Sensor to adjust to the optical characteristics of Airway adapter, to reduce the measurement error. A Zero is necessary only when requested. The following conditions, the system can prevent zero, in order to avoid error correction. Breath is detected in last 20 seconds. If the temperature is not stable.
To perform Zero
1. Connect the EtCO2 Sensor and, wait for the Sensor warm-up message to clear.
2. Connect the airway adapter to the EtCO2 Sensor, and make certain that the airway adapter away from all sources of CO2, including the ventilator, the patient's breath and your own.
3. Set the Host to the zeroing function.
4. Query the status of the EtCO2 Sensor to check that the status bit "EtCO2 Sensor not ready to zero," is not set.
5. Start the Zero. The maximum time for a sensor zero is 40 seconds. The typical time for a zero is 15-20 seconds.
Note: For best results, wait 5 minutes to allow the EtCO2 Sensor to warm up before performing the Zero procedure.
CO2 accuracy check
The following procedure should be performed to check the EtCO2 accuracy of the EXCO2 Sensor. It is recommended that this procedure be performed every 12 months.
1. Attach the EtCO2 Sensor to the Host monitor. Attach a CO2 airway adapter to the EtCO2 Sensor,
2 Tum on the Host monitor
3. On the Host monitor, change to the CO2 Accuracy Mode. This mode will need to display the CO2 waveform value as a numeric instantaneous vabe
4. Wait for the EtCO2 Sensor to warm up to its operating temperature. 5. Set the CO2 Units setting of the EtCO2 Sensor to percent. 6. Set the gas compensation settings of the CO2 Sensor to the verification gas mixture.
7. Zero the ECO2 Sensor.
8. Attach a regulated flowing gas mixture of 5% CO2, balance N2 to the airway adapter. Set the flow rate of the gas to 2 liters per minute. 9. Allow 30 seconds for the gas mixture to stabilize and observe the CO2 value. The expected value is 5% ± 0.26%.
10. If a waveform is present, verify that it appears as a straight line at approximately 5 percent.
11. The accuracy check is now complete. Remember to set the CO2 Sensor settings for units and gas composition back to their previous settings.
Cleaning
Cleaning the EtCO2 Sensor case, Cable and Connector:
1. Clean the EtCO2 Sensor case with a cloth dampened with 70% alcohol.
2. Clean the EtCO2 Sensor case with a clean damp cloth after each use and dry naturally.
Note: Do not immerse or sterilize the Sensor. Note: The Side stream on-airway adapters and side stream sampling kits are single patient use. Treat in accordance with hospital protocols for handling
Airway adapter(single patient use devices.)
EtCO2 Sensor is only used with the airway adapters of Part 5"Sensor and Accessories" in this manual. The airway adapters are intended for single patient use. They are disposable and shall not be re-used. Reuse of single patient use adapters can cause cross infection.
The airway adapters shall be disposed of in accordance with local regulations for bio-hazardous waste. Note: The manufacturer can provide schematics, component lists, legends, calibration details, or other information that helps maintenance personnel repair equipment parts that can be serviced by maintenance personnel authorized by manufacturer.
Specifications
The Mainstream EtCO2 Sensor specifications are subject to change without notice. Unless otherwise stated, all CO2 measurements are made following a zero, with 5% CO2 gas, balance N2 at 25 degrees Celsius, and Pb. = 760 mmHg with 2 liters per minute flow. The stabilization time for full specification testing of the EtCO2 Sensor over the entire temperature range is 20 minutes.
General specifications of this sensor





No comments:
Post a Comment